AllMed partners with healthcare organizations to provide Nurse Review Services, giving them the ability to manage utilization review functions with greater agility and cost-effectiveness. Our team of US-licensed registered nurses (RNs) is dedicated to providing the essential clinical reviewer expertise you need, when you need it, enabling you to focus on your strategic priorities.
Our Nurse Review Services include a comprehensive range of utilization review functions, including prior authorizations of services and procedures, medications, and pre-certifications. We also offer inpatient admission, concurrent reviews, level of care reviews, and continuation of care (inpatient and outpatient) services. With our team of experienced RNs, we can handle a variety of review types and ensure that they are completed efficiently and accurately.
At AllMed, we understand the importance of delivering high-quality clinical review services to healthcare organizations. Our RNs have a deep understanding of healthcare regulations and the healthcare industry, enabling them to provide valuable insights and make informed decisions when reviewing cases. We work closely with our clients to ensure that their specific needs are met and that they receive the best possible service.
Partnering with AllMed provides your organization with a cost-effective solution for managing utilization review functions. By leveraging our Nurse Review Services, you can focus on your strategic priorities while we handle the essential clinical reviewer expertise you need. Our team of experienced RNs is available to assist you with a variety of utilization review functions, ensuring that they are completed quickly and accurately.
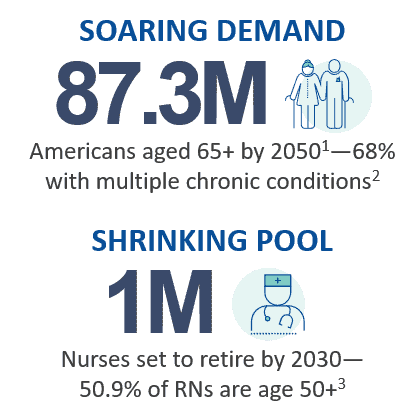
Changing Demand, Fixed Resources for Utilization Reviews
While demand for healthcare services is rising in the U.S.,1,2 the need for specific services can vary from week to week. Given the ongoing U.S. nursing shortage,3 staffing for this variable demand poses significant challenges for payers, health plans, Third-Party Administrators and other payer-centric organizations:
- Additional pressure on turnaround times when case volumes surge
- Mismatch between skills needed and available on staff
- Higher cost of training, retention, and management
- Increased recruitment effort and associated overhead
- Focus on cost reduction as part of a strategic initiative
At AllMed, we designed our Nurse Prior Authorization Review services with these challenges in mind.
How to Quickly Scale to Meet Your Nurse Prior Authorization Review Needs
Our US-licensed RNs work as an extension of your team, integrating seamlessly into your organization. We are here when you need us, enabling you to:
- Deliver accurate reviews securely, efficiently, and in full compliance with URAC, HITRUST, and state and federal regulations
- Meet tight turnaround times when demand surges
- Free your internal resources to focus on strategic priorities
- Improve your RN retention and engagement
- Reduce training, recruiting, and management costs
Our track record speaks for itself—over 98 percent of reviews are delivered within required turnaround times, leading to improved responsiveness and lower overall costs.
Featured Utilization Review Resources

Nurse Review Services
Scale quickly and efficiently when prior authorization, concurrent review, or RN staffing levels fluctuate by partnering with AllMed. Download this brochure to learn how we support your utilization review needs.

Reach Out
Interested in Our Initial Clinical Review Service?
Whether you need access to clinical review expertise or added review capacity,
we’re here to help with customized services that fit your exact needs.

